The healthcare landscape is being reshaped at an unprecedented pace, powered by sophisticated data analytics, emerging technologies, and the escalating demand for real-world evidence (RWE). At the heart of this shift, Health Economics and Outcomes Research (HEOR) harnesses RWE to sharpen clinical decision-making, tailor treatment pathways, and elevate patient care. By embedding authentic, real-world insights into healthcare systems, HEOR is not just adapting to change — it is redefining the future of medical practice. Here’s how:
- Accelerating drug approval and access through real-world data
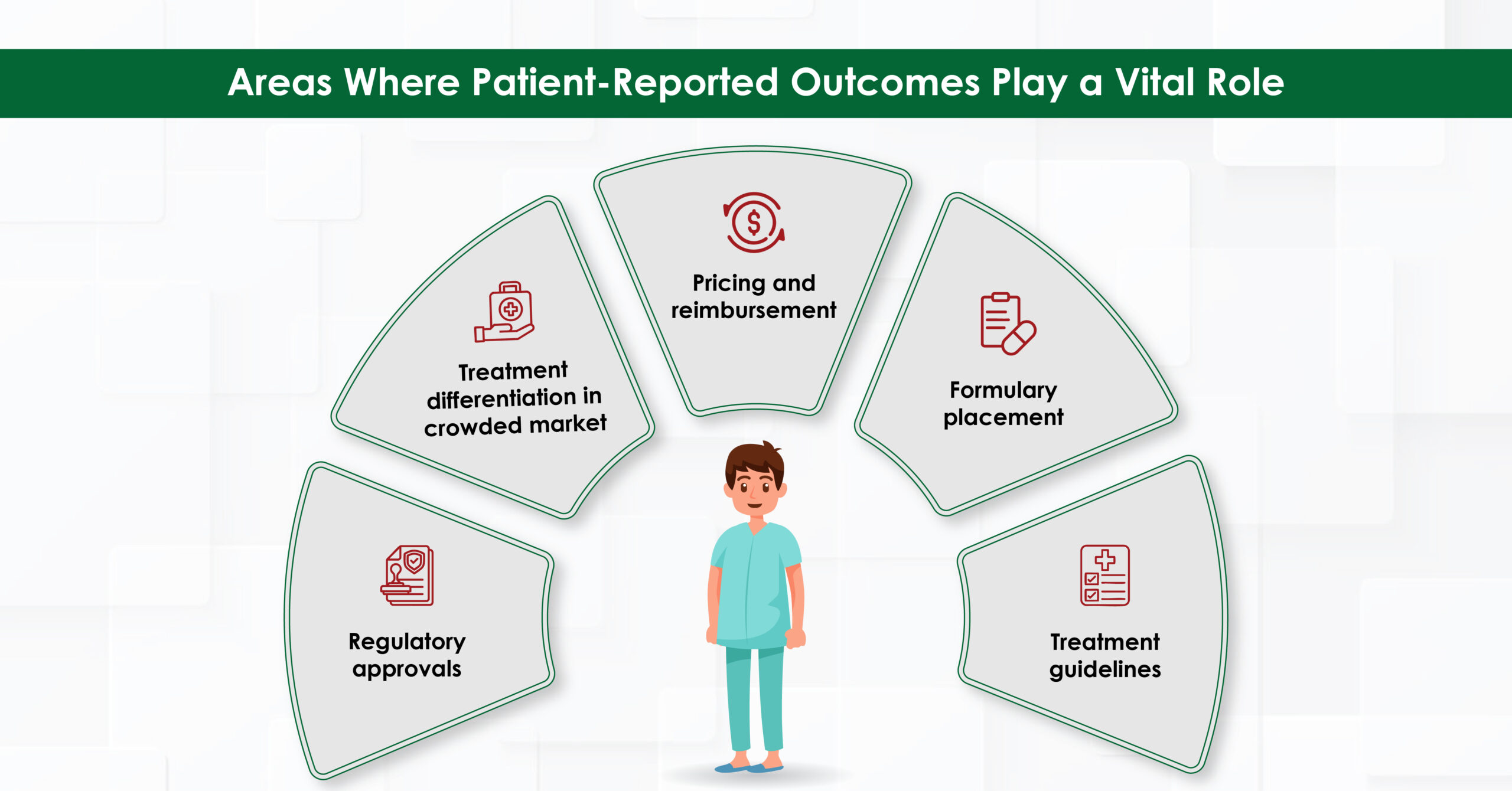
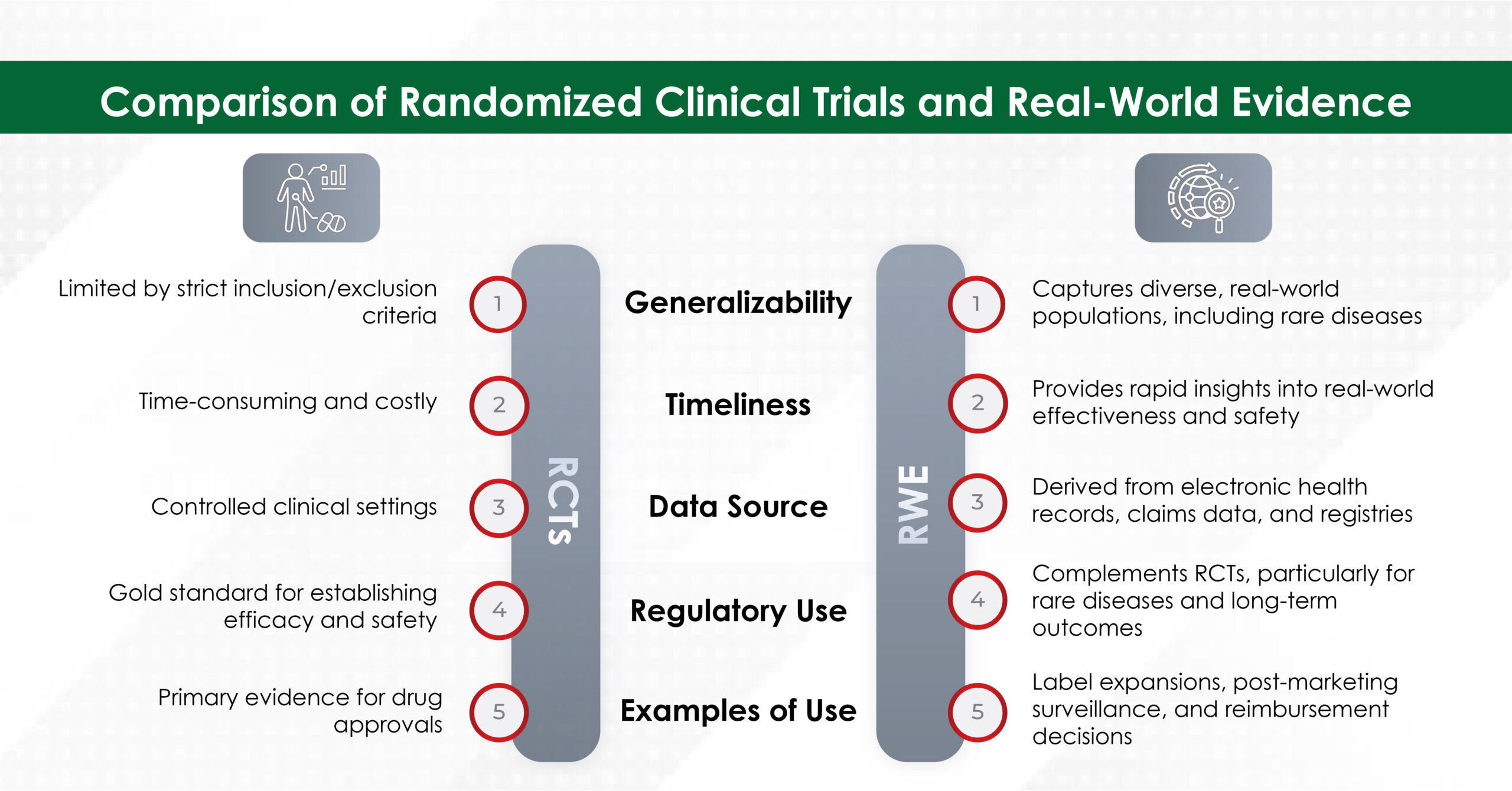
Bringing a new drug to market is a complex and highly scrutinized process. Traditional clinical trials, while essential, often have limitations, such as strict patient selection criteria that may not fully represent real-world populations. HEOR bridges this gap by utilizing RWE to offer a more comprehensive understanding of a drug’s effectiveness and safety across diverse patient groups.
For example, post-marketing RWE studies have been instrumental in demonstrating the long-term efficacy and safety of cancer drugs, helping pharmaceutical companies negotiate with regulators and payers for broader market access.1 By analyzing patient outcomes, healthcare resource utilization, and adherence patterns in real-world settings, HEOR strengthens the case for reimbursement and pricing strategies, ensuring that innovative treatments reach those who need them most.
- Driving value-based care and smarter reimbursement models
The shift from volume-based to value-based healthcare means that reimbursement is increasingly tied to patient outcomes rather than the quantity of services provided. HEOR, supported by RWE, plays a crucial role in assessing the cost-effectiveness and clinical benefits of medical interventions, leading to the adoption of value-based pricing models.
Payers and policymakers rely on HEOR data from sources like electronic health records (EHRs), insurance claims, and patient registries to determine whether treatments justify their costs. For instance, RWE analyses of diabetes treatments have influenced insurance providers to support outcome-based contracts, where reimbursement is tied to patient improvements rather than fixed pricing.2 This approach ensures that high-value treatments are rewarded, reducing inefficiencies and unnecessary healthcare spending.
- Personalizing care with precision insights from RWE
One of the most significant advances in modern medicine is the move toward personalized healthcare. HEOR, powered by RWE, helps identify patient subgroups that benefit most from specific treatments, enabling more targeted and individualized care strategies.
For example, RWE-driven HEOR studies have shown that certain genetic markers can predict a patient’s response to targeted cancer therapies, allowing oncologists to tailor treatment plans accordingly.3 This precision approach minimizes trial-and-error prescribing, reduces adverse events, and improves overall healthcare resource allocation. By aligning therapies with real-world patient data, HEOR enhances the efficiency and effectiveness of medical interventions, leading to better patient outcomes.
- Shaping public health strategies and improving population outcomes
Beyond individual care, HEOR and RWE provide essential insights for population health management and policy formulation. Governments and healthcare providers use this data to craft targeted interventions, address disparities, and respond to public health emergencies.
During the COVID-19 pandemic, HEOR-supported RWE helped evaluate vaccine efficacy across varied populations, guiding immunization strategies worldwide.4 With data-driven policymaking, healthcare systems can allocate resources more effectively and improve health outcomes on a broader scale.
Conclusion
At Turacoz, we aim to integrate HEOR and RWE is revolutionizing healthcare by delivering actionable insights that enhance drug development, refine reimbursement models, personalize treatment approaches, and inform public health strategies. As the healthcare landscape continues to evolve, the role of HEOR in leveraging real-world data will only grow, fostering a more efficient, evidence-driven, and patient-centered healthcare system.
With stakeholders across the healthcare spectrum embracing these advancements, we are moving toward a future where treatments are not only innovative but also accessible, cost-effective, and tailored to patient needs.
How is HEOR transforming healthcare in your region? Join the conversation.
References:
Dang A. Real-world evidence: a primer. Pharmaceutical medicine. 2023 Jan;37(1):25-36.
- Peasah SK, Huang Y, Palli SR, Swart ECS, Donato BMK, Pimple P, et al. Real-world impact of empagliflozin on total cost of care in adults with type 2 diabetes: Results from an outcomes-based agreement. J Manag Care Spec Pharm. 2023 Feb;29(2):152–60. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10387982/
- Agarwala V, Khozin S, Singal G, O’Connell C, Kuk D, Li G, et al. Real-world evidence in support of precision medicine: Clinico-genomic cancer data as a case study. Health Aff (Millwood). 2018 May;37(5):765–72. Available from: https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1579
EUPATI. Real-World Data (RWD) & Real-World Evidence (RWE). EUPATI Toolbox. 2025 Feb 19. Available from: https://toolbox.eupati.eu/resources/patient-toolbox/real-world-data-rwd-real-world-evidence-rwe/