In the field of medical publishing, accuracy and precision are crucial. Medical writers and editors ensure accuracy, clarity, consistency, and error-free information in publications. This task has traditionally been time-consuming and prone to human error. However, with the advent of AI technology, powerful tools to enhance quality control (QC) and copy-editing processes. In this blog, we’ll explore how AI is revolutionizing these crucial aspects of medical publication.
The Challenges of Quality Control and Copy Editing in Medical Publishing
The challenges we face in QC and copy editing for medical publications are varied and can roughly be summed up as:
- Volume and Complexity: Medical literature often involves large volumes of complex information, making thorough review a daunting task.
- Consistency: Maintaining consistency across multiple documents or within large documents can be challenging, especially when multiple authors or editors are involved.
- Technical Accuracy: Ensuring the accuracy of medical terminology, drug names, and statistical data requires specialized knowledge and attention to detail.
- Style Adherence: Different publications may have specific style guidelines that need to be consistently applied.
- Time Constraints: Tight deadlines can put pressure on the QC and editing process, increasing the risk of overlooked errors.
- Cognitive Fatigue: Extended periods of detailed review can lead to mental fatigue, potentially resulting in missed errors.
How AI is Transforming QC and Copy Editing
AI-powered tools have proven to be useful in addressing these challenges, offering solutions that enhance accuracy, efficiency, and consistency in the QC and copy-editing process. Here are some key areas where AI is making a significant impact:
- Automated Proofreading and Grammar Checking
Advanced AI-powered proofreading tools go beyond basic spell-check functionality. They can identify complex grammatical errors, suggest improvements in sentence structure, and even detect nuances in tone and style. For medical writing, these tools can be customized to recognize field-specific terminology and conventions.
Example: Tools like Grammarly or ProWritingAid, when tailored for medical content, can catch errors that might slip past human editors, especially in long documents.
- Consistency Checking
AI can quickly scan entire documents or sets of documents to ensure consistency in terminology, formatting, and style. This is particularly useful for maintaining uniformity across multi-author papers or large clinical trial reports.
Example: An AI tool could flag inconsistencies in the spelling of drug names (e.g., “paracetamol” vs. “acetaminophen”) or variations in formatting of statistical data across a document.
- Reference and Citation Verification
AI-powered reference management tools can automatically check the accuracy and formatting of citations and references. They can also flag potential issues like outdated sources or mismatched citations.
Example: Tools like EndNote or Mendeley now incorporate AI features to suggest relevant citations, check for formatting consistency, and even detect potential citation errors.
- Plagiarism Detection
While not unique to medical publishing, advanced AI-driven plagiarism detection tools are crucial for maintaining the integrity of scientific literature. These tools can identify not just verbatim copying but also paraphrased content and idea similarity.
Example: iThenticate, a widely used plagiarism detection tool in academic publishing, uses AI to compare submitted manuscripts against a vast database of scientific literature.
- Technical Accuracy Checking
Specialized AI tools are being developed to verify the accuracy of medical and scientific content. These can check for correct usage of medical terminology, accuracy of drug dosages, and consistency of statistical reporting.
Example: A hypothetical AI tool could cross-reference drug names and dosages mentioned in a manuscript against established pharmacological databases to flag potential errors or inconsistencies.
- Style Guide Compliance
AI can be trained on specific style guides (e.g., AMA, APA) to ensure that documents adhere to the required formatting and stylistic conventions.
Example: An AI tool could automatically check and correct formatting of headings, tables, and references according to the target journal’s style guide.
- Readability Analysis
AI-powered readability tools can analyze the complexity of the text and suggest simplifications where necessary. This is particularly useful for patient-facing materials or when aiming for clear communication of complex medical concepts.
Example: Tools like Hemingway Editor use AI to suggest ways to make prose clearer and more concise, which can be invaluable for improving the readability of dense medical text.
- Data Consistency and Accuracy Checking
For publications involving large datasets or multiple statistical analyses, AI can verify the consistency and accuracy of reported numbers across text, tables, and figures.
Example: An AI tool could cross-check numerical data in the results section against data presented in tables and figures, flagging any discrepancies for human review.
- Language Translation and Localization
For medical publications that require translation, AI-powered translation tools, when used under human oversight, can significantly speed up the process while maintaining accuracy.
Example: DeepL, an AI translation tool, has shown promising results in accurately translating medical texts, though human review remains essential.
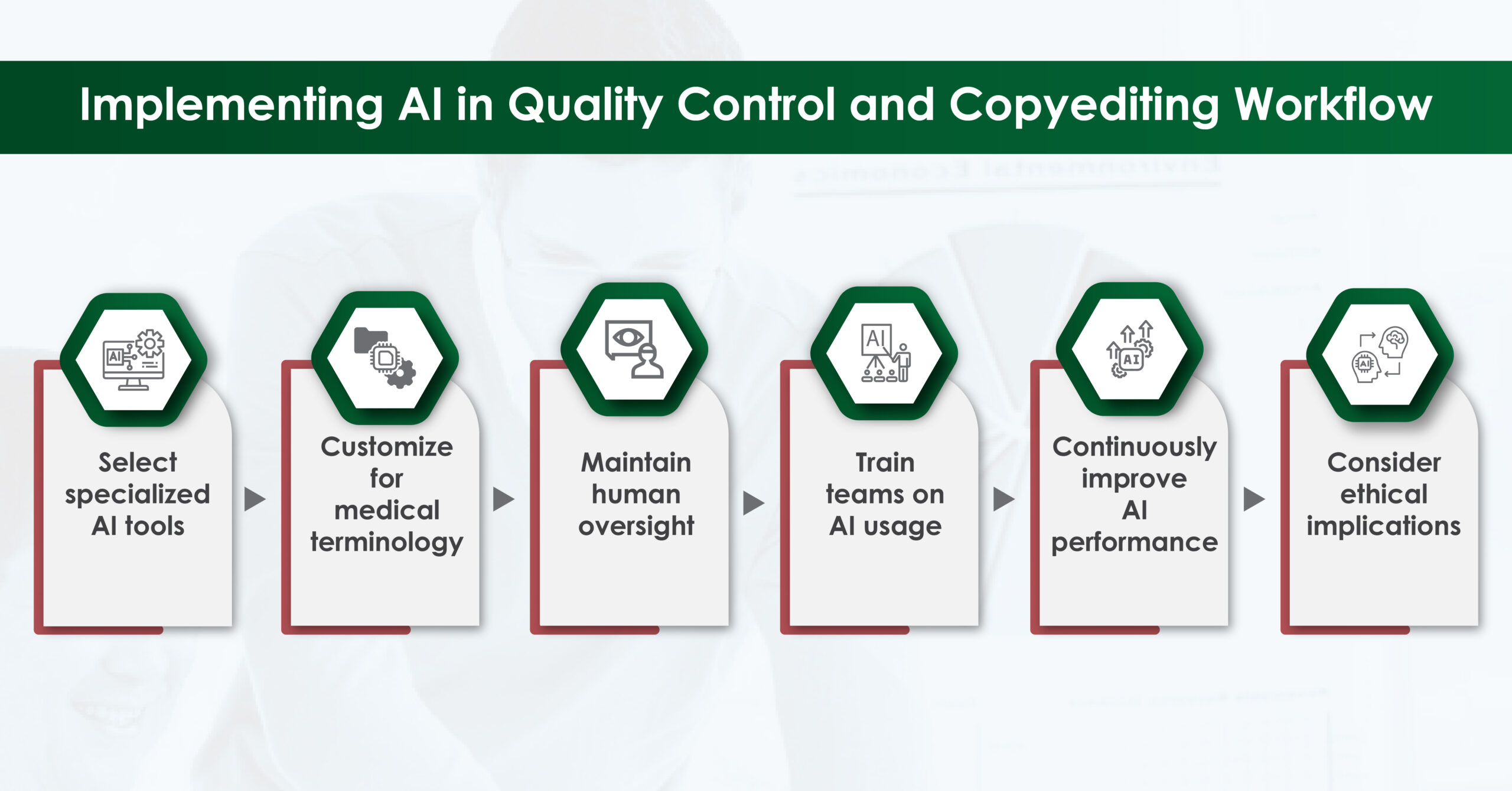
Implementing AI in the QC and Copy-editing workflow
While AI tools offer tremendous potential, their effective implementation requires careful consideration:
Challenges and Limitations
While AI offers significant benefits, it’s important to be aware of its limitations:
- Context Understanding: AI may struggle with nuanced context or highly specialized content. Human expertise remains crucial for interpreting and validating AI suggestions.
- Over-reliance: There’s a risk of becoming overly dependent on AI tools, potentially leading to complacency in human review.
- Learning Curve: Integrating AI tools into existing workflows requires time and may initially slow down processes before improving efficiency.
- Cost: Advanced AI tools can be expensive, potentially limiting access for smaller organizations or individual freelancers.
- Data Privacy: When using cloud-based AI tools, ensure they comply with data protection regulations, especially when handling sensitive medical information.
The Future of AI in Medical Publication QC and Editing
As AI technology continues to evolve, we can expect even more advanced capabilities:
- Predictive Editing: AI might suggest edits based on patterns in previous publications or author preferences.
- Real-time Collaboration: AI could facilitate real-time editing and QC in collaborative environments, flagging potential issues as content is being created.
- Automated Fact-Checking: Advanced AI might cross-reference claims in manuscripts against current medical literature to flag potential inaccuracies or outdated information.
- Enhanced Contextual Understanding: Future AI may better understand complex medical contexts, reducing false positives and improving suggestion relevance.
AI technology is revolutionizing quality control and copy editing in medical publishing. By leveraging these tools, we can significantly enhance the accuracy, consistency, and efficiency of our work. However, it’s crucial to remember that AI is a powerful assistant, not a replacement for human expertise. The most effective approach is to combine the strengths of AI – speed, consistency, and the ability to process vast amounts of data – with the nuanced understanding, contextual knowledge, and critical thinking of human medical writers and editors.
As we move forward, embracing and adapting to these AI technologies will be key to maintaining the highest standards in medical publishing. By doing so, we can focus more of our human efforts on the aspects of our work that truly require our unique insights and expertise, ultimately leading to higher-quality medical publications and, by exten