Biosimilars—biologic medicines that are highly similar to FDA-approved originator biologics—offer a cost-effective alternative without compromising clinical efficacy.1,2 Since the first U.S. biosimilar approval in 2015, however, their market adoption has progressed more slowly than expected, despite a steady increase in FDA approvals and their proven safety and effectiveness.3,4 Payers have been cautious in fully embracing biosimilars, even though they are pivotal in reimbursement decisions and prescribing patterns. Understanding the barriers to biosimilar adoption and exploring how Health Economics and Outcomes Research (HEOR) can address these challenges is crucial for unlocking the full potential of biosimilars in transforming healthcare access and affordability.
Why Are Payers Hesitant to Adopt Biosimilars?
Several key challenges slow biosimilar adoption among payers:4
- Lack of confidence in interchangeability: Payers often demand robust safety and efficacy data to feel comfortable substituting originators with biosimilars
- Limited financial incentives: Without clear cost savings or reimbursement benefits, payers may not prioritize biosimilar uptake
- Administrative burdens: Complex approval processes involved in switching the treatments can deter payers from encouraging biosimilar use
These concerns have created a cautious environment, slowing down the transition from originator biologics to biosimilars. This is where HEOR plays a pivotal role by generating comprehensive evidence that addresses payer concerns through cost-effectiveness analyses (CEA), budget impact models (BIMs), and real-world evidence (RWE).
How HEOR Supports Biosimilar Adoption
- Cost-Effectiveness Analysis (CEA)
The value of biosimilars, in comparison to originator biologics, can be assessed through CEA, which considers both their lower costs and comparable clinical efficacy.
For instance, CEA conducted in Canada for the treatment of metastatic colorectal cancer found that the biosimilars MVASI® and Zirabev® offered annual cost savings of €6379 compared to the originator drug, Avastin, without compromising survival outcomes. The study also supported the initial policy decision to mandate using bevacizumab biosimilars over the originator formulation. This approach helped reduce budget allocation toward bevacizumab and facilitated more efficient resource allocation while maintaining effective care.5 These savings highlight the potential for biosimilars to reduce healthcare expenditures without compromising patient outcomes.
- Budget Impact Models (BIMs)
While CEAs assess value, BIMs estimate the actual financial consequences of adopting biosimilars on healthcare systems. BIMs help payers understand potential cost savings and resource allocation implications, which are critical for reimbursement decisions.
The practical impact of BIMs is evident in several European countries. The introduction of biosimilar adalimumab and tocilizumab across seven European nations—including the UK, Germany, and France—was projected to yield cumulative savings of €462 million and enable treatment for an additional 65,593 patients.6 Similarly, a U.S. study on biosimilar adalimumab showed that faster conversion rates from originator to biosimilar led to greater savings, with cumulative savings reaching $28.8 million in a fast-conversion scenario.7 This demonstrates that not only the decision to adopt biosimilars but also the speed of adoption impacts financial outcomes.
- Real-World Evidence (RWE)
By leveraging RWE, researchers can better understand the clinical effectiveness and safety of biosimilars outside the structured environment of clinical trials. This data is crucial in building payer confidence by demonstrating that biosimilars perform similarly to originators in everyday clinical practice.
For instance, a real-world population-based study in British Columbia found no significant differences in healthcare resource utilization or clinical outcomes between biosimilar and originator etanercept users.8 This evidence helped underpin the province’s biosimilar switching policy. This policy dramatically increased biosimilar prescriptions: etanercept and infliximab biosimilar use rose by 76.98% and 58.43%, respectively. The switch generated substantial cost savings and improved patient access to biologic therapies without compromising safety or efficacy.9
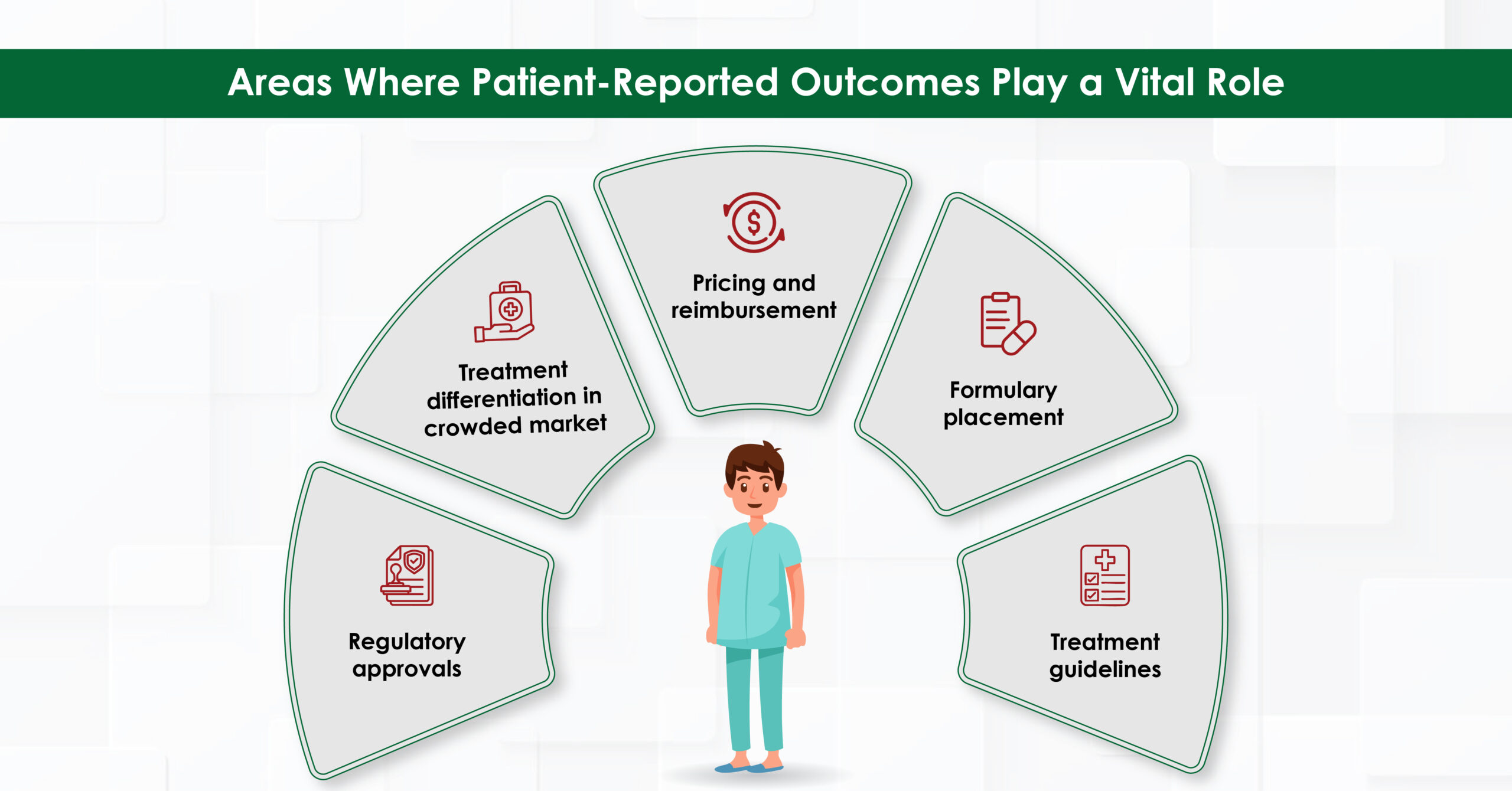
How HEOR Influences Payer Decisions
HEOR evidence directly informs payer strategies in several ways:
Practical Influence
- Cost Savings: Payers are motivated by the potential for significant cost reductions. For example, EU-5 markets saved €303.86 million with biosimilar rituximab.10 These savings can be reinvested to expand patient access or improve healthcare services.
- Reimbursement Policies: HEOR informs the design of reimbursement frameworks, including price discounts, tendering processes, and mandatory switching policies. Countries like the UK and Germany have successfully implemented these strategies, which have been instrumental in driving biosimilar uptake.11,12
Theoretical Influence
- Value-Based Healthcare: HEOR aligns with value-based healthcare principles by prioritizing interventions that deliver optimal outcomes at the lowest cost. Biosimilars exemplify this approach by reducing treatment costs without compromising quality.13
- Policy Formation: Policymakers use HEOR findings to shape regulations encouraging biosimilar use. British Columbia’s biosimilar switching policy is a prime example, where evidence-based policy led to increased biosimilar uptake and substantial cost savings.9
Conclusion
In conclusion, as the healthcare system faces mounting pressures to deliver high-quality care while managing costs, adopting biosimilars stands out as a compelling opportunity that cannot be ignored. The collaborative efforts of regulators, payers, and providers, guided by robust HEOR evidence, are key to ensuring that the transition from originators to biosimilars is clinically sound and economically advantageous. HEOR has provided clear insights into cost-effectiveness, budget impact, and real-world performance, enabling payers to make informed decisions, optimize reimbursement strategies, and contribute to forward-thinking policy development. Ultimately, HEOR’s role in biosimilar adoption is not just supportive but transformative, paving the way for a more sustainable and accessible healthcare future.
References:
- Yang J, et al. Greater uptake, an alternative reimbursement methodology needed to realize cost-saving potential of oncology biosimilars in the United States. J Manag Care Spec Pharm. 2021;27(12):1642-1651.
- Mroczek DK, et al. Obstacles to Biosimilar Acceptance and Uptake in Oncology: A Review. JAMA Oncol. 2024;10(7):966-972.
- Shubow S, et al. Prescriber Perspectives on Biosimilar Adoption and Potential Role of Clinical Pharmacology: A Workshop Summary. Clin Pharmacol Ther. 2023;113(1):37-49.
- Edgar BS, et al. Overcoming barriers to biosimilar adoption: real-world perspectives from a national payer and provider initiative. J Manag Care Spec Pharm. 2021;27(8):1129-1135.
- Lu B, et al. Cost-Effectiveness Analysis of Bevacizumab Biosimilars Versus Originator Bevacizumab for Metastatic Colorectal Cancer: A Comparative Study Using Real-World Data. Value Health. 2024;27(12):1689-1697.
- Shastri K, et al. AB1428 Adalimumab and Tocilizumab Biosimilars in Europe: Budget-impact and Opportunity for Expanded Patient Access. Ann Rheum Dis. 2024;83:2069-70.
- Chaplin S, et al. Budget impact analysis of including biosimilar adalimumab on formulary: A United States payer perspective. J Manag Care Spec Pharm. 2024;30(11):1226-1238.
- Lacaille D, et al. POS0874 Comparable Safety and Effectiveness Among New Users of Biosimilar vs Originator Anti-NFTs in Inflammatory Arthritis: Population-based Evidence From a Policy Change. Ann Rheum Dis.;83:595-6.
- McClean AR, et al. Uptake and Spending on Biosimilar Infliximab and Etanercept After New Start and Switching Policies in Canada: An Interrupted Time Series Analysis. Arthritis Care Res (Hoboken). 2023;75(9):2011-2021.
- Jang M, Simoens S, and Kwon T. Budget Impact Analysis of the Introduction of Rituximab and Trastuzumab Intravenous Biosimilars to EU-5 Markets. BioDrugs. 2021;35(1):89-101.
- Zhang W, et al.
- Machado S, et al. Policy measures and instruments used in European countries to increase biosimilar uptake: a systematic review. Front Public Health. 2024;12:1263472.
- Chen HH, Yemeke T, and Ozawa S. Reduction of biologic pricing following biosimilar introduction: Analysis across 57 countries and regions, 2012-19. PLoS One. 2024;19(6):e0304851.